Mercola: Fauci must be fired and arrested
11/15/2021 / By News Editors

STORY AT-A-GLANCE
- Vitamin D optimization is likely the easiest, least expensive and most fundamental beneficial strategy that anyone can do to minimize their risk of COVID-19 and other infections
- October 31, 2020, I published a scientific review in the journal Nutrients, co-written with William Grant, Ph.D., and Dr. Carol Wagner. Our paper is the second-most downloaded study from this journal in the past 12 months. It’s also No. 2 in citations for articles in the past 12 months, and No. 4 for views
- The study with the most downloads in the past year and the all-time highest number of views is another vitamin D paper, which found vitamin D supplementation reduced the risk of influenza and COVID-19 infections and deaths
- A third vitamin D paper nabbed the No. 1 spot for most-cited study in the past 12 months. This study found vitamin D supplementation improved survival in frail elderly hospitalized with COVID-19
- To improve your immune function and lower your risk of viral infections, you’ll want to maintain a vitamin D level between 60 ng/mL and 80 ng/mL (150 nmol/L and 200 nmol/L). Vitamin D optimization is particularly important for dark-skinned individuals, as the darker your skin, the more sun exposure you need to raise your vitamin D level, as well as the elderly
(Article by Dr. Joseph Mercola republished from Articles.Mercola.com)
October 31, 2020, I published a scientific review1 in the journal Nutrients, co-written with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel.
This paper, “Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity” — which you can download and read for free — is the second most downloaded study from this journal in the past 12 months.
Our paper is also No. 2 in citations for articles in the past 12 months, and No. 4 for views. Article metrics reveal it’s been viewed 131,458 times as of November 2, 2021, with a daily average of 62 views. The second and third most-viewed articles were also on vitamin D for COVID.
The study with the most downloads in the past year, at 62,590 downloads, and the all-time highest number of views (178,562) is another vitamin D paper2 by Bhattoa et.al., which found vitamin D supplementation reduced the risk of influenza and COVID-19 infections and deaths. The coauthors of my paper, Grant and Baggerly, were coauthors on this paper as well.
A third vitamin D paper, by Annweiler et. al., also nabbed the No. 1 spot for most-cited study in the past 12 months. This study found vitamin D supplementation improved survival in frail elderly hospitalized with COVID-19.
All of this is incredibly encouraging, and demolishes the ridiculous claim that there’s “no scientific basis” for the recommendation of vitamin D for COVID. Indeed, as of September 27, 2020, data from 14 observational studies — summarized in Table 1 of our paper3 — indicate vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19.
What’s more, the evidence generally satisfies Hill’s criteria for causality in a biological system4 (i.e., strength of association, consistency of evidence, temporality, biological gradient, plausibility or mechanism of action, and coherence, although coherence still needs to be verified experimentally).
Mechanisms of Action
As explained in our paper, having sufficient vitamin D in your system can reduce your risk of COVID-19 and other respiratory infections via several different mechanisms, including but not limited to the following:5
| Reducing the survival of viruses |
| Inhibiting the replication of viruses6 |
| Reducing inflammatory cytokine production |
| Maintaining endothelial integrity (endothelial dysfunction contributes to vascular inflammation and impaired blood clotting, two hallmarks of severe COVID-19) |
| Increasing angiotensin-converting enzyme 2 (ACE2) concentrations — Angiotensin II is a natural peptide hormone that increases blood pressure by stimulating aldosterone. ACE2 normally consumes angiotensin I, thereby lowering the concentration of angiotensin II. However, SARS-CoV-2 infection downregulates ACE2, resulting in excessive accumulation of angiotensin II, which worsens the infection |
| Boosting your overall immune function by modulating your innate and adaptive immune responses |
| Reducing respiratory distress7 |
| Improving overall lung function |
| Helping produce surfactants in your lungs that aid in fluid clearance8 |
From my perspective, vitamin D optimization is one of the easiest, least expensive and most impactful strategies to reduce your risk of serious SARS-CoV-2 infection and other respiratory infections.
Vitamin D optimization is particularly important for dark-skinned individuals (who tend to have lower levels than Caucasians unless they spend extended time in the sun), the elderly, and those with preexisting chronic health conditions.
All of these are also risk factors for COVID-19, so population-wide optimization of vitamin D levels could significantly improve COVID outcomes among the most vulnerable.
Vitamin D also lowers your risk of several major chronic killers and comorbidities associated with poor COVID-19 prognosis, including obesity,9 Type 2 diabetes,10 high blood pressure11 and heart disease.12 All of these factors make it an important component of COVID-19 prevention and treatment.
Vitamin D helps prevent these conditions largely because it is a fat soluble steroid hormone that penetrates nearly every cell in your body and passes into the nucleus to affect the optimization of 2,000 to 3,000 genes to create a healthier you.
Vitamin D Is a Key Component for Optimal Immune Function
While the official narrative is now that the human body is defenseless without gene-based intervention (i.e., mRNA or DNA-based COVID injections), anyone still able to think clearly will recognize the nonsense of that argument. The truth is, your body is well-equipped to handle just about any infection, provided your immune system is working properly, as that is your body’s first line of defense.
Vitamin D receptors are found in a large number of different tissues and cells, including your immune cells. This means vitamin D plays an important role in your immune function specifically. If vitamin D is lacking, your immune system will be impaired, which in turn makes you more susceptible to infections of all kinds.
In the video at the top of this article, Dr. Roger Seheult reviews how vitamin D works, and its benefits, both for respiratory infections in general and as it pertains to COVID-19. Importantly, vitamin D is a steroid hormone that can pass through cellular membranes into the nucleus and controls the expression of genes. So, it’s not just a mere vitamin required as a cofactor. It can actually modify how the cells in your body behave and function. As noted by Seheult, vitamin D:
- Stimulates “the innate immune response, which provides frontline protection against infectious agents”
- Increases expression of antimicrobial peptides in your monocytes and neutrophils — both of which play important roles in COVID-19
- Enhances expression of an antimicrobial peptide called human cathelicidin, “which is of specific importance in host defenses against respiratory tract pathogens”
Higher Vitamin D Levels Lower Risk of COVID Infection
While Seheult also reviews a number of studies looking at vitamin D in relation to respiratory illnesses other than COVID-19, SARS-CoV-2-specific investigations have found that COVID-19 is far more common in vitamin D deficient individuals.
In one study,13,14,15 82.2% of COVID-19 patients tested were deficient in vitamin D, compared to 47.2% of population-based controls. (Mean vitamin D levels were 13.8 ± 7.2 ng/ml, compared to 20.9 ± 7.4 ng/ml in controls.)
They also found that blood levels of vitamin D were inversely correlated to D-dimer levels (a measure of blood coagulation). Many COVID-19 patients have elevated D-dimer levels, which are associated with blood clots. Vitamin D has also been linked to a lower risk of testing positive for COVID-19 in the first place.
The largest observational study16 to date, which looked at data for 191,779 American patients, found that of those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested positive for SARS-CoV-2, compared to 8.1% of those who had a vitamin D level between 30 and 34 ng/ml (adequacy) and only 5.9% of those who had an optimal vitamin D level of 55 ng/ml or higher. According to the authors:
“SARS-CoV-2 positivity is strongly and inversely associated with circulating 25(OH)D levels, a relationship that persists across latitudes, races/ethnicities, both sexes, and age ranges.”
Vitamin D Status Influences COVID-19 Severity
COVID-19 patients who have higher vitamin D levels also tend to have milder illness and better outcomes overall. One study17,18 found the risk of severe COVID-19 and related deaths virtually disappeared when vitamin D levels were above 30 ng/mL (75 nmol/L).
In another study,19 COVID-19 patients with a vitamin D level between 21 ng/mL (50 nmol/L) and 29 ng/mL (75 nmol/L) had a 12.55 times higher risk of death than those with a level above 30 ng/mL. Having a level below 20 ng/mL was associated with a 19.12 times higher risk of death.
Our vitamin D paper20 also lists data from 14 observational studies that show vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19. This is quite logical, considering vitamin D regulates inflammatory cytokine production — a lethal hallmark of COVID-19 — and is an important regulator of your immune system.
Seheult also reviews studies showing COVID-19 outcomes appear to be linked to UVB exposure. For example, in one such study,21 they found a marked variation in mortality depending on whether the patients lived above or below 35 degrees North latitude. As noted by the authors:22
“… the hypothesis is not that vitamin D would protect against SARS-CoV-2 infection but that it could be very important in preventing the cytokine storm and subsequent acute respiratory distress syndrome that is commonly the cause of mortality.”
How to Optimize Your Vitamin D Level
While conventional medicine insists a vitamin D level of about 20 ng/mL is adequate, that really only applies for bone health. For optimal health, immune function and disease prevention, you want a blood level between 60 ng/mL and 80 ng/mL year-round. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L.
If you live in a sunny locale and practice sensible sun exposure year-round, you might not need any supplements. The DMinder app23 is a helpful tool to see how much vitamin D your body can make depending on your location and other individual factors.
I walk on the beach for about an hour a day, wearing only shorts and a cap — and no sunscreen, as it filters out the ultraviolet rays that trigger vitamin D production — and haven’t needed oral supplementation for over a decade. (Keep in mind that the only way to ensure your sun exposure is enough is to get tested, ideally twice a year, in summer and winter.)
Many, unfortunately, don’t get enough sun exposure for one reason or another, and in these cases, an oral vitamin D supplement may be required. Just remember that the most important factor here is your blood level, not the dose, so before you start, get tested so you know your baseline.
Here’s a quick summary of how to determine whether you might need an oral supplement, and your ideal dosage:
1.First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit. Once you know what your blood level is, you can assess the dose needed to maintain or improve your level.
2.Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5. To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.24
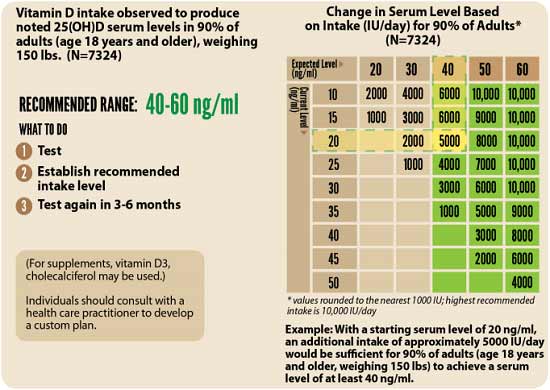
3.Retest in three to six months — Lastly, you’ll need to remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
Simple Way to Improve Your Vitamin D Absorption
Keep in mind that the specific dosage required to maintain an optimal vitamin D level can vary widely from person to person depending on a variety of factors, including skin pigmentation, age and weight. Your gut health can also play an important role in how well you absorb the vitamin D you take.25
When you have a healthy gut, beneficial bacteria produce butyrate by breaking down dietary fiber. Butyrate, in turn, helps increase vitamin D, so the more butyrate you have, the more vitamin D your body can absorb.
Another factor that can influence your vitamin D absorption is your magnesium level.26 Magnesium is required for the conversion of vitamin D into its active form.27,28,29,30 According to a scientific review31,32 published in 2018, about half of Americans taking vitamin D supplements may not get significant benefit as the vitamin D simply gets stored in its inactive form, and the reason for this is because they have insufficient magnesium levels.
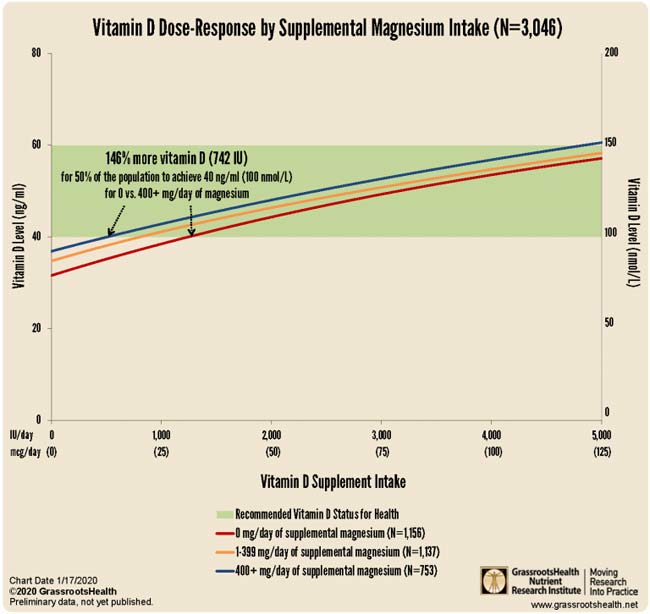
Research by GrassrootsHealth33 shows you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
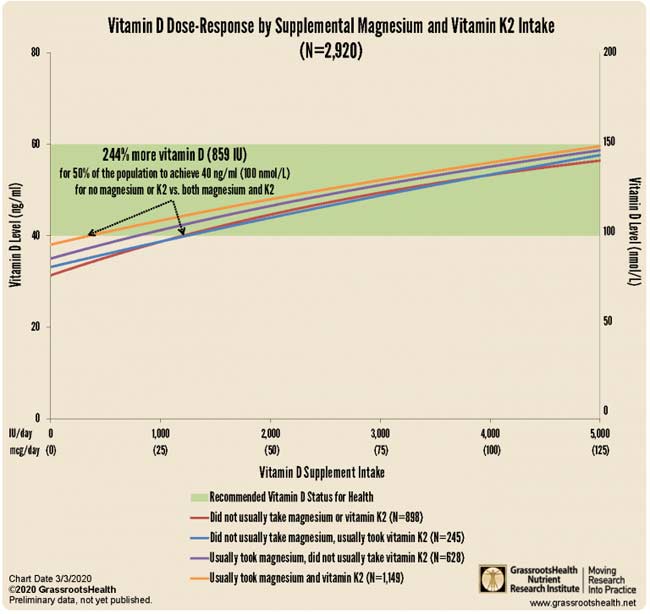
Your vitamin K2 intake can also affect your required vitamin D dosage. According to GrassrootsHealth,34 “combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,” and “those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither.”
Data35 from nearly 3,000 individuals revealed 244% more oral vitamin D was required to get 50% of the population to achieve a vitamin D level of 40 ng/ml (100 nmol/L) if they weren’t concurrently also taking magnesium and vitamin K2. So, a simple way to optimize your vitamin D absorption is to take it in conjunction with magnesium and K2.
Read more at: Articles.Mercola.com
Submit a correction >>
Tagged Under:
biological weapons, biowar, coronavirus, COVID, COVID treatment, deaths, Fauci, health, prevention, SARS-CoV-2, vaccines, vitamin D
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
MedicalTyranny.com is a fact-based public education website published by Medical Tyranny Features, LLC.
All content copyright © 2018 by Medical Tyranny Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.