Study shows children are typically prescribed two antibiotics for pneumonia unnecessarily, with no proven additional benefit in health outcomes
08/31/2018 / By Zoey Sky

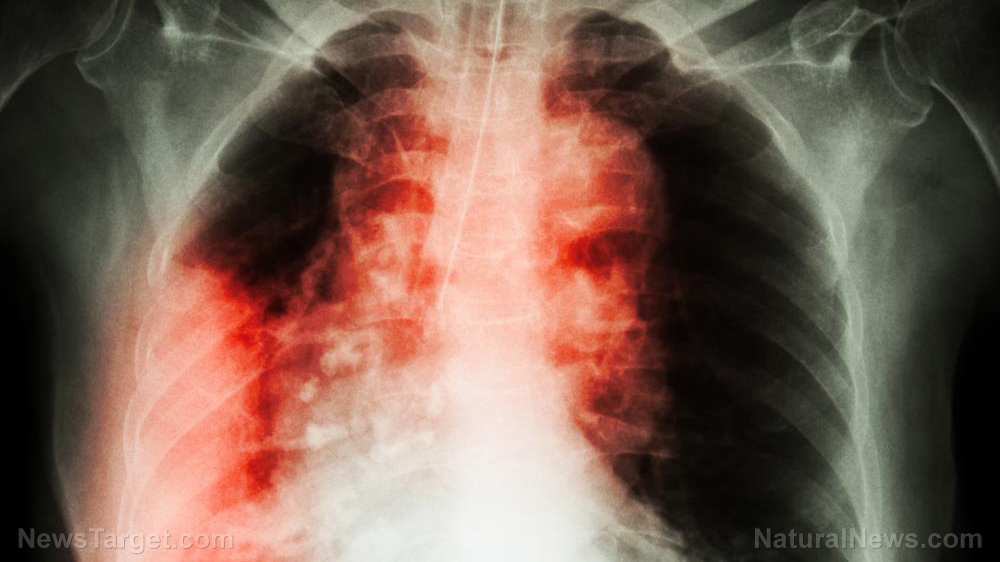
Antibiotic resistance is an alarming trend, and according to a JAMA Pediatrics study, the combination of two antibiotics usually “prescribed to treat community-acquired pneumonia in children” is unnecessary. The use of a single antibiotic is often all a patient needs.
Researchers from Vanderbilt University Medical Center have revealed that administering amoxicillin on its own is a better option compared to combining it with azithromycin. Simply decreasing the number of drugs administered can help minimize the instances of antibiotic resistance across the country. (Related: White kids take twice as many antibiotics as other kids, putting them at higher risk, study finds.)
Azithromycin, an antibiotic often prescribed by pediatricians, “accounted for almost 20 percent of all antibiotic prescriptions for children in the U. S. ambulatory setting,” as per an editorial that was published along with the study.
Derek Williams, M.D., MPH, assistaonia and other respiratory illnesses” is a step towards stalling the worrisome “progression of antimicrobial resistance.”
nt professor of Pediatrics, and lead author, said, “Combination therapy with azithromycin is unnecessary in most cases of pediatric pneumonia, both because the bacteria targeted by azithromycin are less common than other causes of pneumonia, including viruses, and the effectiveness of azithromycin has not been clearly demonstrated in prior studies.” He adds that healthcare professionals can do their part to curb antibiotic resistance by decreasing exposure to antibiotics whenever they can to ensure that currently available antibiotics remain effective.
Williams et al. observed 1,418 children, made up of 693 girls and 725 boys, who were hospitalized for “radiologically confirmed community-acquired pneumonia.” A beta-lactam antibiotic called amoxicillin was given to 72 percent of the study patients, and 28 percent were administered both amoxicillin and azithromycin.
The “length of stay, intensive care admission, readmissions or recovery at follow-up” among the two groups of patients were not drastically different, proving that “combined therapy” isn’t a more effective option compared to administering just amoxicillin.
Williams cautions that amoxicillin or ampicillin, its IV equivalent, is often the preferred treatment for the most common bacteria that cause pneumonia. Meanwhile, azithromycin is administered to patients infected with atypical pneumonia bacteria such as including Mycoplasma pneumoniae. He adds that even though atypical infections are more common “in older children and adolescents,” the benefits of addressing these infections aren’t as apparent.
Williams comments that compared to other conditions, the bulk of antibiotic days in American children’s hospitals are attributed to pneumonia, making it a “hugely important target for antimicrobial stewardship efforts.” Making conscious efforts to minimize “unnecessary antibiotic use in pediatric pneum
According to Kathryn Edwards, M.D., professor of Pediatrics and the Sarah H. Sell and Cornelius Vanderbilt Chair and co-author of the study, their work has pointed out the significant role of viruses when it comes to pneumonia. She concluded that the results of their study can help point healthcare providers to the ideal antibiotics that will be used to cure bacterial pneumonia.
However, parents and guardians need to vigilant when it comes to a prescription for antibiotics that are given to their children. Whenever possible, opt for natural alternatives that do not have any dangerous side effects.
Natural alternatives to antibiotics
If you want to do your part to curb antibiotic resistance, try some of these natural alternatives to antibiotics:
- Garlic – A natural antibiotic, garlic has potent antibiotic, antiviral, anti-fungal, and antimicrobial properties. It can also help protect and facilitate the removal of unfriendly bacteria.
- Oil of oregano – Oil of oregano gets rids of pathogenic bacteria without disrupting beneficial bacteria. It is also antiviral and anti-fungal, making it a powerful natural antibiotic.
- Echinacea – A potent herb, echinacea is often used for colds and flu because it can destroy the most dangerous forms of bacteria such as staphylococcus aureus, which causes the deadly methicillin-resistant Staphylococcus aureus (MRSA).
- Manuka honey – When applied topically, manuka honey can kill various pathogens like MRSA and flesh-eating bacteria.
You can learn more about superfoods and other natural cures at Cures.news.
Sources include:
Tagged Under: amoxicillin, ampicillin, antibiotic resistance, Antibiotics, atypical pneumonia bacteria, azithromycin, beta-lactam antibiotic, children's health, Combination therapy, drugs, harmful medicine, Mycoplasma pneumoniae, Pneumonia